Thoughts on telehealth payments
This month marks five years since the World Health Organization declared Covid-19 a pandemic. It’s been half a decade since life as we know it ground to a halt, and we all became much more dependent on telehealth.
Though in-office medical care today is not as restricted as in 2020, we continue reaping the benefits of early pandemic expansions and innovations in telehealth. One of the pandemic’s biggest upsides was how this expansion opened up new, virtual avenues to specialist care for many patients who would otherwise find it challenging to access.
One of the areas where telehealth has especially exploded is mental health. In theory, virtual care should have helped us distribute access to mental health care more evenly across populations that need it.
However, as with much of healthcare, the way mental health—including virtual counseling—is paid for determines much of how it functions and whom it benefits.
Here’s a potent example: I recently came across a study of New York telehealth reimbursement policy and its downstream impacts.
- The research suggests that the way telehealth payments are designed may be hurting the facilities serving patients who need virtual care the most.
- Telehealth reimbursements for Medicaid patients seen by providers at so-called federally qualified health centers (FQHCs) fall by about one-third when the provider doesn’t come into the office.
- However, coming into the office just to see patients over video calls is massively challenging to incentivize. Mental health providers know they earn more seeing patients virtually from home for non-FQHCs.
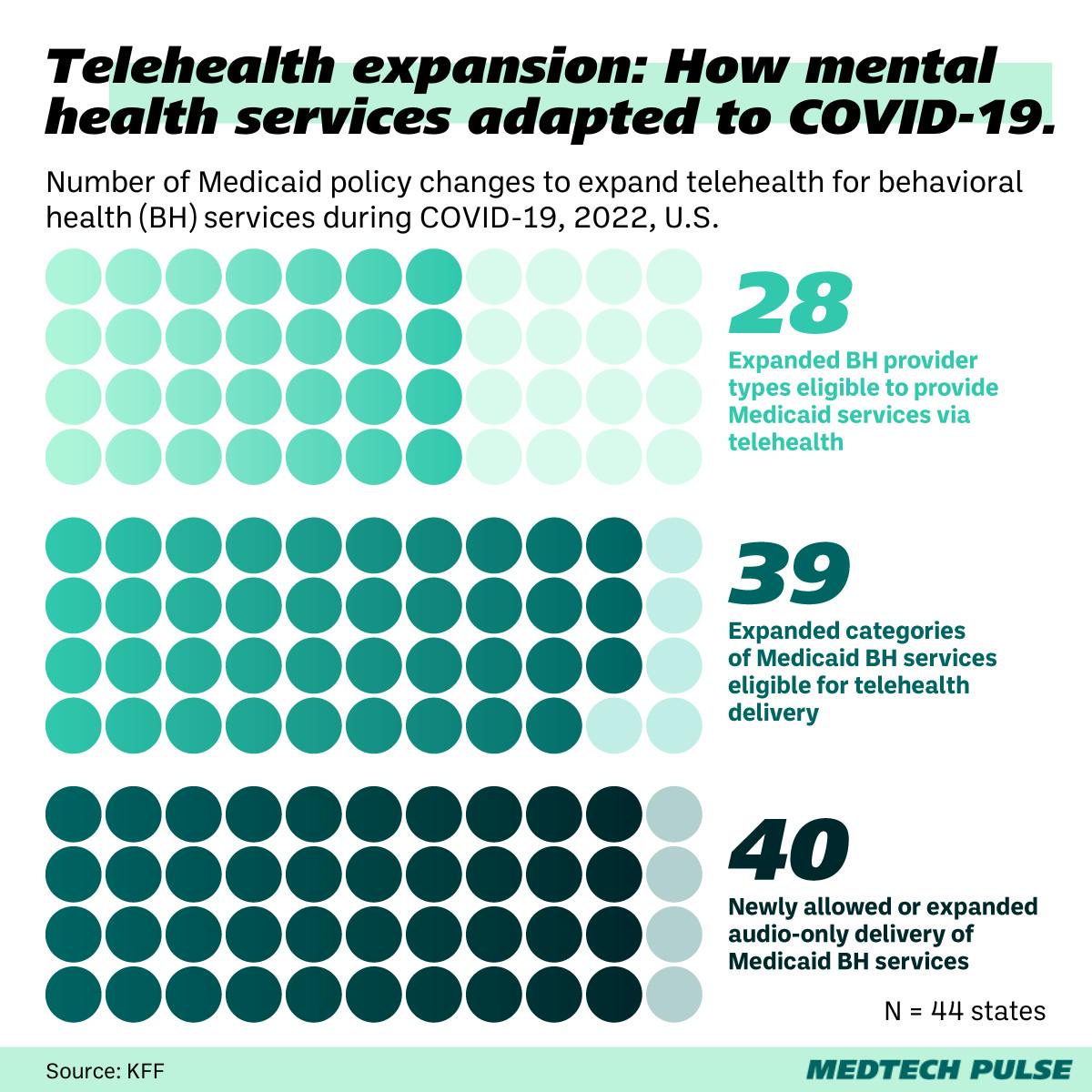
Just a few years ago, when we envisioned all that the rise of telehealth could do for us, many of us rejoiced at the improvements in healthcare access this new status quo would surely bring. In the U.S., state expansion of Medicaid (the program that funds care for lower-income Americans, people with disabilities, and many children) took off nationwide, especially for behavioral health coverage.
And yet, the rules of that coverage, as we see from that study, don’t quite align with how providers actually practice.
It’s an important reminder that medtech innovation is both hampered and enabled by policy design. We medtech proponents must keep that in mind as we bring products to market and as we advocate for policies that favor medtech adoption. That’s how we ensure providers and patients actually benefit.
