CT Scans: New innovations increase the diagnostic power of a familiar medical technology
In MedTech Pulse, we tend to cover the latest developments in medical technology: new discoveries and inventions are our bread and butter.
But today, we’re here to discuss a technology that has been around for over half a century: The computed tomography (CT) scan.
British engineer Godfrey Hounsfield used the first-ever CT scan of a human brain on October 1, 1971. His initial inspiration for developing the approach was the question of how archaeologists may be able to detect hidden areas in Egyptian pyramids.
In the 21st century, CT scans are a common tool in medicine. The modern scans use a combination of x-rays and computer imaging to visualize the inside of patients’ bodies for a variety of diagnostic reasons — ranging from investigating internal injuries to diagnosing tumors.
We’re discussing CT scans not to look back on the history of medical innovation (though we do think stories like Hounsfield’s are fascinating). We’re excited to explore the ways medtech breakthroughs are increasing the way this common medical technology can help diagnose and treat more conditions.
Two papers published this past month explore how CT imaging can continue being on the forefront of medical breakthroughs — decades after its initial invention. Let’s take a look.
CT imaging and AI to predict lung cancer risk
A new study shows that, with just one CT scan, AI predicts lung cancer risk 6 years into the future.
MIT researchers developed an AI model that can use the results of a single CT scan to predict patients’ risk of developing lung cancer up to six years into the future.
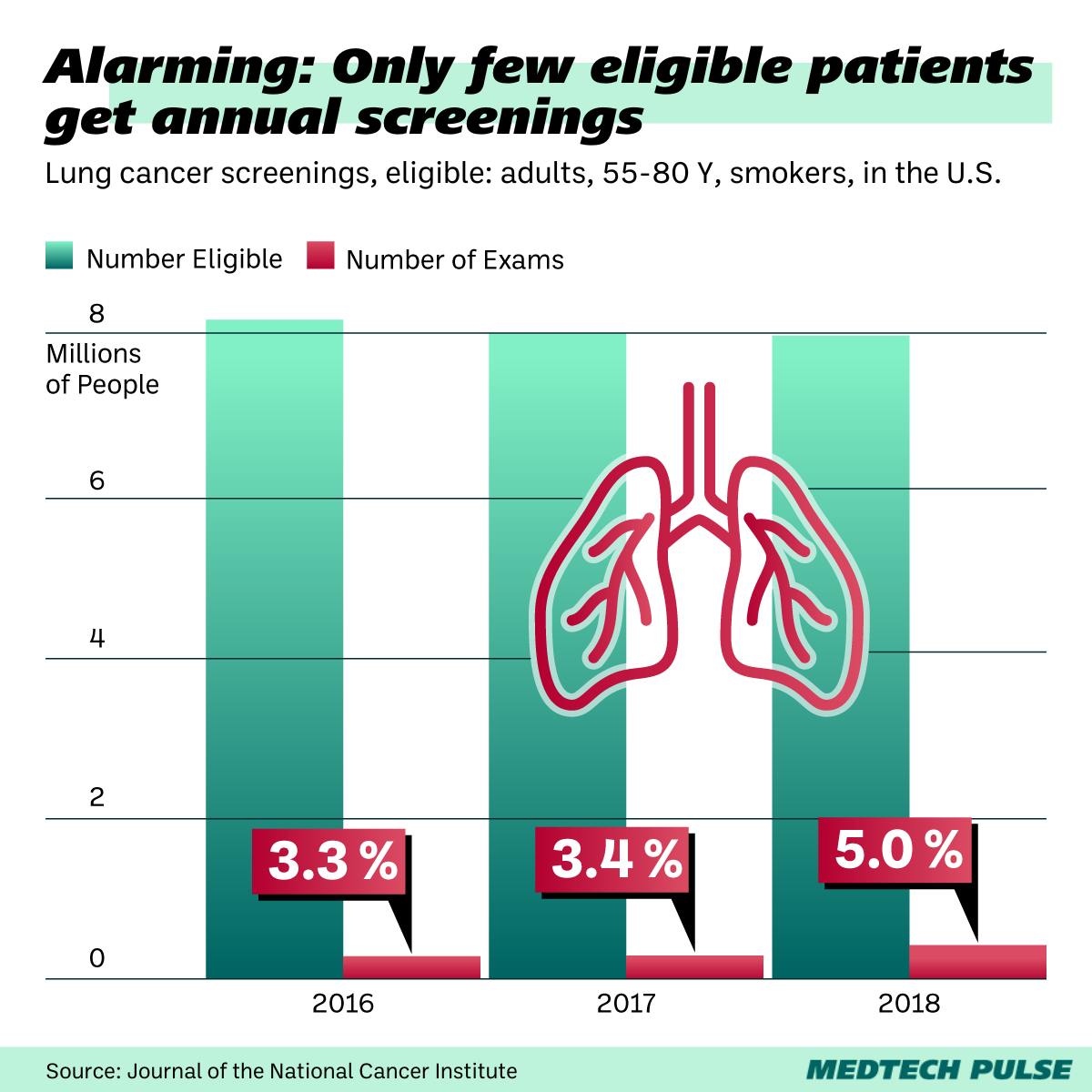
Why is this such a breakthrough? Currently, the U.S. recommends annual LDCT scans for those aged 50+ with a 20-pack-per-year history of smoking. However, surveys have shown that less than 10% of the eligible population is getting annual screenings.
Furthermore, those being screened are not being optimally followed-up with to encourage repeat screening. Thus, more personalized, predictive screening might go a long way for patients who may tend to screen more sporadically or rarely.
The researchers have made the model freely available at clinics for research use. With this action, they aim to validate their research findings in subpopulations under-represented in the original research.
They also hope to examine how the technology can fit into the real-world context of clinical practice.
With this approach, they make a prudent step toward ensuring the viability of the eventual application of their innovation by providers (which can be a tricky part of the innovation process, as we discussed in our last issue).
CT scans as a new, less-invasive tool for treating hypertension
Another novel application of CT imaging explores the scan as a new method to evaluate a hypertension procedure.
A new study has demonstrated that CT scans are at least as accurate at predicting the outcomes of a hypertension procedure as the current standard, invasive approach.
The patients who may benefit from this development have primary aldosteronism (PA), a type of hypertension caused by an adrenal gland nodule producing a steroid hormone. PA currently accounts for 20–25% of treatment-resistent hypertension cases.
This isn’t because PA is untreatable. In fact, certain PA patients can undergo a surgical resection of the nodule to treat their hypertension. The procedure used to differentiate between operable and inoperable PA cases, AVS, is invasive and rarely offered by hospitals.
Thus, many PA patients do not have access to a potential cure.
The Queen Mary University of London team behind the research study identified that metomidate positron emission tomography (MTO), a type of CT scan, can serve as a new way to diagnose unilateral PA — the operable kind of PA.
In the study, MTO was found to be at least as accurate as AVS.
But hypertension patients and providers can’t celebrate quite yet. While MTO scans are more easily available in hospitals, the radioactive tracer involved in the procedure has a 20-minute half-life — it needs to be synthesized on site and used immediately.
However, alternative tracers with a longer half-life are in clinical development. Perhaps, in the near future, this study’s findings will be able to help more patients improve their blood pressure.
The takeaway: new medtech need not always be entirely “new”
To us, the lesson from these two fascinating publications is clear. Sometimes, the best medtech innovation is applying existing, widely available, and reliable technology in novel, more efficient ways.
Yes, novel technologies like AI present an exciting new frontier in our industry. Yet, the technology that can most readily help patients and providers is often the one they have the easiest access to and applicable knowledge of right now.
Thus, we celebrate medical technology’s history. And not only because it brings us exciting tales of how Ancient Egypt connects to modern oncology.
We see the past as a source of inspiration and tangible material for the most readily implementable future innovations.