Renegade AI company helps patients fight claim denials
“Make your health insurance company cry too.”
That’s the pitch on the homepage of startup FightHealthInsurance.com’s website. The company was started by software engineer Holden Karau, who created it from the frustration she felt while recovering from a car accident, when she was repeatedly denied coverage for physical therapy.
AI vs AI: FightHealthInsurance.com is just one of the players in what STAT is calling an “emerging arms race”: the use of AI in the world of health insurance.
- UnitedHealth, the health company that made headlines perhaps more than any other last year, is currently being sued for alleged misuse of AI in claim denials.
- However, they’re not the first to do it. Back in 2023, Medicare Advantage plans were already being investigated for their use of AI in senior citizens’ claim denials. And a recent U.S. Senate inquiry found that CVS/Aetna too relied heavily on AI in increasing claim denials.
- With algorithms increasingly being wielded by commercial payers to manage claims, patient and provider advocates like Karau are also turning to AI to fight back.
A new area of healthtech innovation: Karau is not alone in her fight against wrongful claim denials. About $36 million has been raised by a handful of companies in this space over the past few years.
Other companies serving patients and providers in this space include:
- Banjo Health — a prior authorization platform built for clinicians and health plans
- Crosby Health — an appeals automation platform for clinicians
- ParX Solutions — a prior authorization platform for clinicians and patients
- CoFactor AI — an appeals automation platform for clinicians
- Guardian AI — an appeals automation platform for clinicians
- Claimable — a generative AI platform helping patients file appeals
In the pharmacy benefits space, similar organizations include CoverMyMeds and eBlu Solutions.
AI for public good: Beyond seizing on a moment of public outcry against these practices, these innovators are working to wield AI as many other technologists intend: They see a cumbersome, inefficient process and they work to automate it.
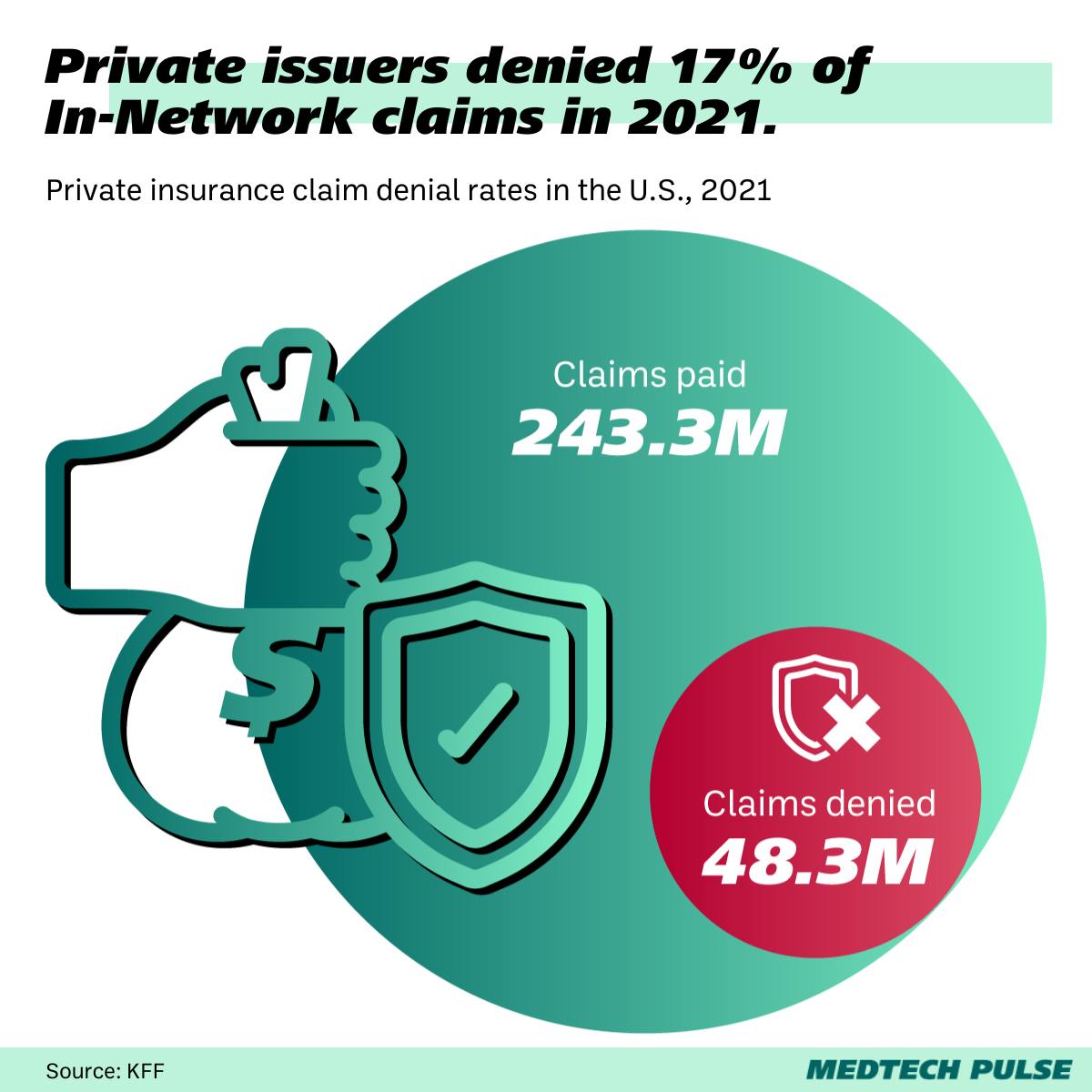
- Private insurance companies issue tens of millions of claim denials each year in the U.S.
- Though they have the right to, patients rarely appeal these denials. This is despite the fact that appeals are often successful.
- These patient- and provider-focused innovators’ hope is that, in making filing an appeal much easier, more providers will retain their revenue and more patients will feel empowered to fight for their right to healthcare.